Do you feel a sharp pain in your heel when you take your first step in the morning? The cause could be plantar fasciitis, a common foot complaint.
Your feet endure tremendous stress with every step you take. The stress is even higher if you do high-impact activities, such as running. So it’s not surprising your feet hurt from time to time, and one of the most common causes of foot pain is plantar fasciitis.
Nearly 1 million patients are treated each year for plantar fasciitis, a painful foot condition causing intense heel pain. The pain can be so severe it can make exercise and even simple motions like walking difficult. If left untreated, plantar fasciitis can lead to knee and back pain.
Plantar fasciitis is often seen in active adults, such as long-distance runners. Yet it can develop in anyone who stands on their feet all day on hard surfaces, such as teachers or factory workers. The good news is that plantar fasciitis is reversible with conservative therapies. The podiatry specialists at New York Bone & Joint Specialists have the diagnostic expertise and treatment skills to help you get the spring back in your step.
What is Plantar Fasciitis?
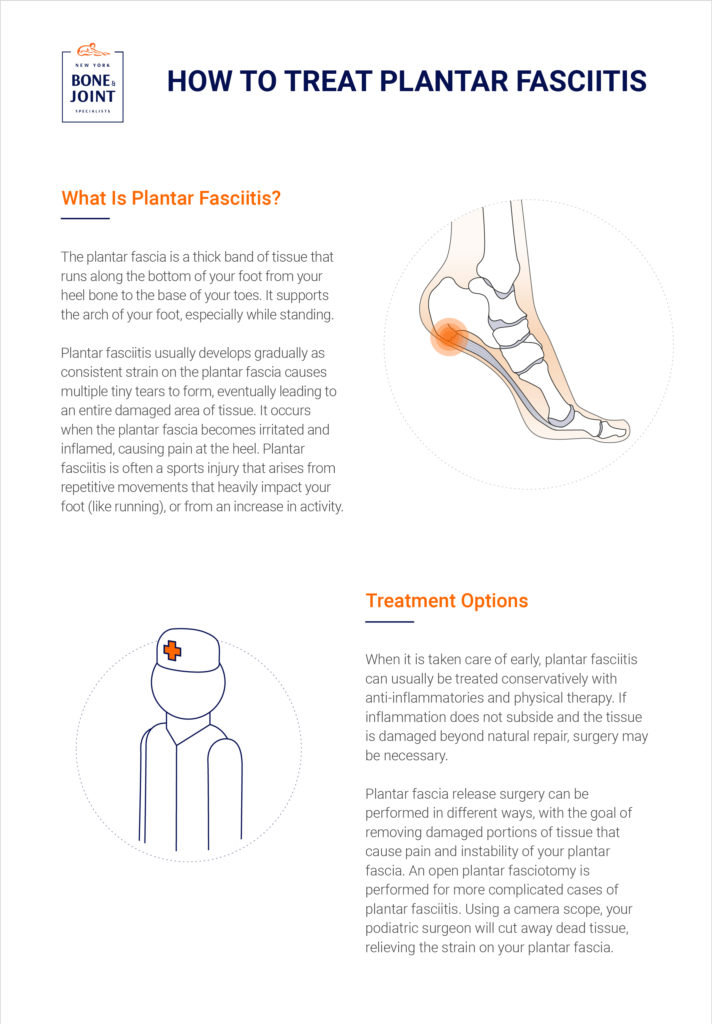
Running along the bottom of your foot is the plantar fascia, a tough, fibrous stretch of tissue connecting your heel to your toes. It supports your arch when you stand, but also enables you to flex your foot when you walk or run.
Because our feet absorb a significant amount of force during a typical day, the plantar fascia can develop microtears and inflammation. The tissue is also vulnerable to stress from repetitive actions, such as pounding the pavement when running.
Plantar fasciitis symptoms gradually progress, starting with occasional heel pain (especially when waking) to chronic discomfort when walking if left untreated. The condition tends to strike older adults between the ages of 40 to 60.
Plantar Fasciitis Symptoms: Recognizing the Signs
Although plantar fasciitis symptoms may develop over time, the condition exhibits these noticeable pain patterns:
- Sharp pain centered in the heel or the arch of the foot
- Unable to flex the foot due to stiffness
- Severe pain when taking the first step in the morning
- Pain after a period of rest, such as when standing up after sitting
- Pain diminishes during exercise or movement, but intensifies when resting
What Causes Plantar Fasciitis?
These risk factors can cause plantar fasciitis:
- Biomechanical. High or flat arches; tight calf muscles or Achilles tendon; overpronation (a defect in your gait causing your arches to flatten when you walk or run).
- Activity-related. Repetitive movements in running or dancing.
- Lifestyle factors: Obesity or working at jobs requiring prolonged standing on hard surfaces (factory workers, teachers).
- Footwear. Shoes with thin or no arch support (sandals, flip-flops, worn-out athletic shoes).
- Age. Active adults aged 25 to 65, peaking between 40 and 60.
- Previous foot injury. An untreated heel spur could irritate the plantar fascia.
Conservative Treatment Options for Plantar Fasciitis
Plantar fasciitis symptoms can be resolved within weeks with conservative methods, such as:
- Rest and activity modifications. Rest your foot for a week and switch to low-impact exercises, such as biking and swimming.
- Ice therapy. Cover a frozen water bottle with a thin towel and roll it under your foot for 10 to 15 minutes twice a day to ease inflammation.
- Stretching exercises. Focus on stretching the calf muscles and the plantar fascia.
- Pain management. Take over-the-counter non-steroidal pain relievers (aspirin, ibuprofen, naproxen) for 10 days.Talk to your doctor if they don’t relieve the pain and you need stronger medication.
- Night splints. Your foot relaxes as you sleep, which causes morning heel pain. Although it can take getting used to, a splint worn at night stretches the plantar fascia, thereby reducing heel pain.
- Physical therapy. A physical therapist can show you effective stretches and massage techniques to loosen foot and calf muscles.
- Walking boot. A walking boot takes pressure off the foot. Your doctor will tell you how long to wear it.
- Corticosteroid injections. An anti-inflammatory medication such as a steroid is injected into the plantar fascia. But the number of shots is limited due to potential tissue damage.
- Orthotics. Custom-made or commercially available inserts lift the heel, support the arch, and ease pressure on the plantar fascia.
When is Plantar Fasciitis Surgery Necessary?
The vast majority of plantar fasciitis symptoms ease with conservative treatments. If symptoms have not subsided in six to 12 months, plantar fasciitis surgery followed by physical therapy may be an option.
Types of surgery for plantar fasciitis:
Gastrocnemius recession
- Recommended when a tight calf muscle is causing the plantar fasciitis
- One of the calf muscles is lengthened to relax the plantar fascia and enable the foot to flex
- Can be done as an open surgery or endoscopically
- After surgery, you’ll wear a boot and recovery will take six to eight weeks
Plantar fascia release
- Reserved for patients who can move their ankle but still have heel pain
- The surgeon cuts a portion of the fascia ligament to release tension in the tissue
- If done as an open surgical procedure, recovery will take up to six weeks with a walking boot worn for three weeks
- Recovery will be shorter with minimally invasive endoscopic surgery
Complications are rare but may include nerve damage and failure to relieve pain.
“That stabbing heel pain when you take your first steps in the morning is your body’s way of telling you that your plantar fascia needs attention. We specialize in non-invasive treatments that address the root cause of your plantar fasciitis, helping you walk, run, and stand comfortably again.” – Dr. Leon Popovitz, MD, New York Bone & Joint Co-Founder.
Best Shoes for Plantar Fasciitis: Footwear Solutions
Look for these features in the best shoes if you have plantar fasciitis:
- Arch support: Firm arch support distributes pressure evenly across the foot and prevents overpronation
- Cushioned heel: Good cushioning softens the impact on the heel as you walk
- Deep heel cup: Stabilizes your heel and keeps your foot aligned
- Rigid or semi-rigid midsole: Prevents the foot from bending too far and straining the plantar fascia
- Proper fit: The shoe should hold the heel in place and have adequate toe space
- Insert compatibility: Whether an athletic or dress shoe, the footwear should allow enough room for an orthotic insert
Plantar Fasciitis Prevention Strategies
Medical intervention at the first signs of heel pain can improve your chance of a shorter, successful recovery. But plantar fasciitis can be prevented if you follow these tips:
- Get the right footwear. Look for shoes with good arch support, with a moderate to low heel, and extra cushioning. Don’t wear flats, flip-flops, or walk barefoot.
- Toss out worn shoes. Replace sneakers or athletic shoes every six to nine months, or when the soles wear out.
- Stretch. Stretch your calf muscles and plantar fascia before and after exercise, especially if you run.
- Lose weight. Relieve pressure on the plantar fascia by shedding extra pounds.
- Change your exercise routine. For a short period, stop high-impact activities that stress the foot, such as running. Switch to lower intensity workouts, ranging from cycling and swimming to using an elliptical machine.
Workplace considerations for standing jobs:
- Avoid standing for long periods on hard surfaces; take short breaks and sit.
- Wear supportive footwear with inserts.
- Stand on anti-fatigue mats if you stand on concrete or other hard surfaces.
Advanced Treatment Options
In addition to conservative therapies and surgery, New York Bone & Joint Specialists offers advanced techniques for plantar fasciitis treatment:
- Platelet-rich plasma (PRP) therapy: Uses platelets from the patient’s own blood to restore soft tissue. The platelets are extracted from the patient’s blood and then injected into the plantar fascia to promote healing.
- Extracorporeal shock wave therapy (ESWT): Reserved for chronic plantar fasciitis that hasn’t responded to conservative treatments. Sound waves are pulsed into the heel to stimulate healing.
- Ultrasound-guided tissue repair: In this minimally invasive procedure, a needle-like probe is guided by ultrasound imagery into the affected plantar fascia to break up damaged tissue.
- Stem-cell therapy: Harvests the body’s stem cells to regenerate damaged tissue. The cells are obtained from the hip bone, concentrated, and then injected into the affected area.
Why choose us for Plantar Fasciitis surgery in NYC?
New Yorkers have trusted our plantar fasciitis doctors and surgeons for decades. We are recognized as leaders in the field due to our:
- Commitment to Joint Health: We prioritize the health and healing of your joints, understanding their vital role in an active and fulfilling life.
- Comprehensive & Compassionate Care: Our world-class specialists provide expert, empathetic guidance from diagnosis through rehabilitation.
- Effective Non-Surgical Solutions: Over 90% of plantar fasciitis cases are successfully resolved through our orthopedic treatments, often avoiding surgery.
- Dedication to Your Full Recovery: We are committed to your complete recovery, utilizing conservative methods and only resorting to expert surgical intervention when absolutely necessary.
NYC’s Top-Rated Plantar Fasciitis Specialists
At New York Bone & Joint Specialists, our philosophy centers on preserving your body’s natural structures, particularly for long-term foot health. This commitment to exceptional care means 90% of our patients recover without surgery, ensuring lasting health and function, and offering peace of mind.
Make an appointment today
Ready to take the first step toward relief? Schedule an appointment with New York Bone & Joint Specialists and start your personalized recovery plan today.
Plantar Fasciitis: FAQs
What are the first signs of plantar fasciitis?
The first sign of plantar fasciitis is a sharp pain in the heel upon the first step in the morning. The pain may lessen when walking or running, but returns at rest. Without early treatment, the pain can become chronic and lead to knee and lower back pain.
What type of doctor should I see for plantar fasciitis?
A podiatrist, orthopedist, or foot surgeon is qualified to treat plantar fasciitis. Luckily, New York Bone & Joint offers top-rate specialists in plantar fasciitis treatment and other foot disorders.
What are the best shoes for plantar fasciitis relief?
The best shoes for plantar fasciitis are those with good arch support and cushioning around the heel. The shoe should hold the heel in place and allow enough room for an orthotic insert, if needed.
How do I find a plantar fasciitis doctor near me?
Look for board-certified orthopedists with fellowship training in podiatry. At New York Bone & Joint Specialists, our foot specialists are trained in both conservative methods to relieve foot pain. We suggest surgery only when necessary.
When is surgery needed for plantar fasciitis?
Plantar fasciitis responds well to non-surgical treatments. When conservative methods fail to bring relief, surgery may be a viable option.
What shoes should I avoid with plantar fasciitis?
Avoid shoes with no arch support, such as sandals or flip-flops. Wearing worn-down sneakers or athletic shoes with thin insoles increases the risk of plantar fasciitis.
Is plantar fasciitis the same as heel spurs?
No. A heel spur, or a bony growth where the fascia connects to the heel bone, may develop if plantar fasciitis goes untreated for a long time. But you might not feel any pain directly from a spur. Instead, the heel pain is the result of plantar fasciitis, not the spur.










