GLUTEUS MEDIUS PAIN
What causes it and what can you do?
If you’re feeling recurring pain at the side of your hip, you might have a torn gluteus medius. This muscle is attached to the greater trochanter, the bony protrusion at the side of the hip, and runs along the upper end of the hip. The gluteus medius is responsible for abduction, or the lateral movement of the legs from the body, and ensures that we stand straight and don’t limp while walking.
Occurring after the muscle is torn from the greater trochanter, a tear in the gluteus medius prevents patients from walking properly, causing sharp pain and inflammation at the side of the hip whenever they attempt to put weight on the affected leg. The extent and severity of the condition will vary from patient to patient.
GLUTEUS MEDIUS TEAR SYMPTOMS
Common symptoms of a gluetus medius tear include:
- Pain and inflammation at the side of your hip
- Weakness in that area if severely damaged
- Pain when sitting or moving your leg
- Warmth, tenderness, or redness in the affected area
Your orthopedic specialist can diagnose a gluteus medius tear by raising your leg away from your body to target the area of tenderness and weakness.
An MRI may be useful in determining the extent of tissue damage. It will reveal if your tendon is stretched or torn, which may require surgery if your pain and weakness are severe enough.
GLUTEUS MEDIUS TEAR PAIN RELIEF
While a torn gluteus medius can cause considerable pain, there are some readily available treatments for immediate pain relief. In most cases, anti-inflammatory medications will alleviate the swelling and reduce the pain. Icing and gentle stretching can also provide relief.
TREATMENT FOR A TORN GLUTEUS MEDIUS
Treatment for gluteus medius tears will vary based on the extent and severity of the injury.
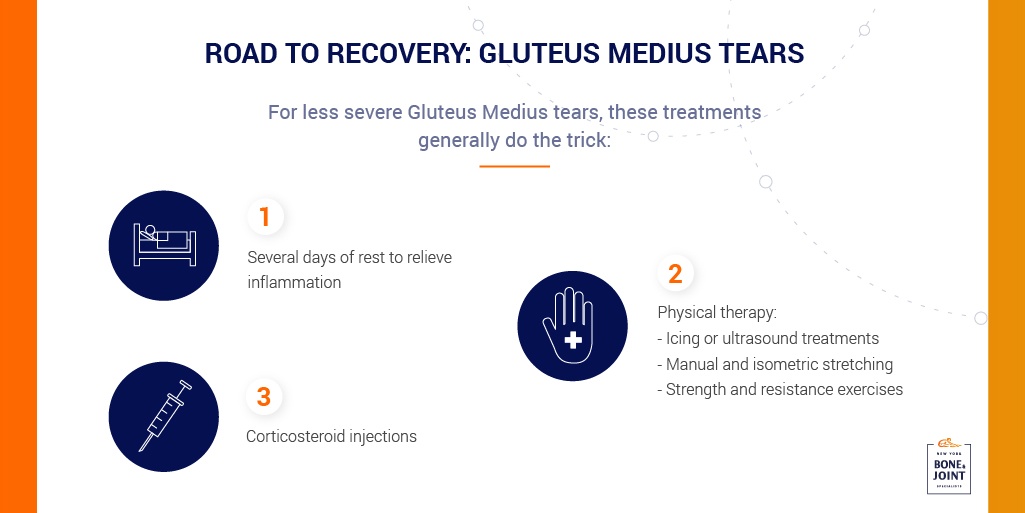
In less severe cases, your orthopedic specialist will generally recommend several days of rest to relieve inflammation and irritation before beginning physical therapy. Your physical therapy regimen will likely be accompanied by a course of oral anti-inflammatories and a corticosteroid injection into the hip trochanteric bursa to alleviate pain during your recovery.
The therapy itself will likely consist of icing or ultrasound treatments to calm inflammation, manual and isometric stretching to relieve stiffness and increase blood flow to the affected muscle, and, after several weeks, strength and resistance exercises designed to rebuild muscle mass and restore mobility.
If pain persists after three to six months of these more conservative treatments, your gluteus medius may need to be surgically repaired. Surgery is generally necessary only when the tendon has been permanently lengthened or torn and cannot provide stability for the hip.
Most gluteus medius tears can be repaired arthroscopically. The procedure entails several incisions into the skin surrounding the muscle through which the surgeon views the torn muscle and operates on it, sewing the tendon back in place, removing permanently damaged tissue, and making other needed repairs. This outpatient procedure generally leads to a quick recovery period and greatly reduces the risk of scarring or other complications.
While most gluteus medius tears respond to these courses of treatment, more severe ruptures may need to be repaired with an open surgery during which your surgeon will use anchors to stabilize the repaired tendon. Open surgery has a longer recovery time, and patients will need more intense physical therapy to regain a complete range of motion.
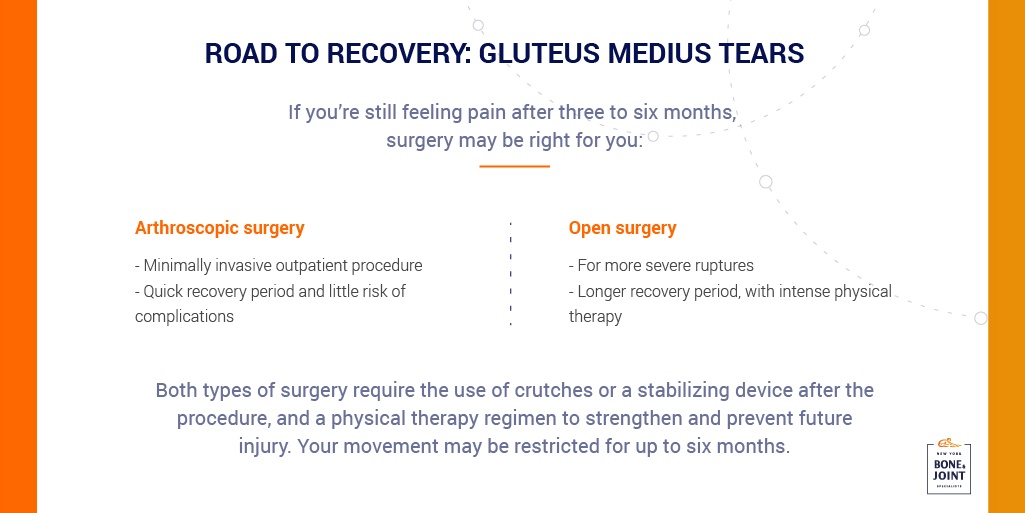
After surgery (whether arthroscopic or open), you will need to walk with crutches or a stabilizing device strapped onto your hip so that the repaired tissues do not become stretched out. While your movement will be restricted for at least six months, you will begin physical therapy within several weeks of surgery to stretch the gluteus medius. Physical therapy exercises will help keep the hip from stiffening, increase your range of motion, and prevent the growth of scar tissue. Later you’ll engage in strengthening exercises to support the healing hip and prevent future injury to the weakened tendon.
Regardless of the severity of your tear, our seasoned specialists at New York Bone and Joint are committed to offering you the best in orthopedic care. With your long-term health in mind, we aim to ensure that you receive the most effective course of treatment. Schedule an appointment with one of our specialists today to receive a formal diagnosis.
Frequently Asked Questions About Gluteus Medius Tears
What does a gluteus medius tear feel like?
A gluteus medius tear typically causes sharp, localized pain on the side of your hip, particularly over the bony prominence (greater trochanter). The pain often worsens when you try to bear weight on the affected leg, walk, climb stairs, or move your leg away from your body. You may experience a noticeable limp or find yourself leaning to one side when standing to avoid putting pressure on the injured hip.
Many patients describe tenderness, warmth, or even redness in the affected area. Unlike general hip soreness from overuse, a gluteus medius tear creates a specific, persistent pain that doesn’t improve with rest alone. You might also notice weakness when trying to lift your leg to the side or difficulty standing on one leg. The pain can radiate down the outer thigh and may be worse at night, especially when lying on the affected side.
If you’re experiencing these symptoms, particularly after a fall, sudden movement, or gradual onset with repetitive activities, it’s important to see an orthopedic specialist for proper diagnosis.
How is a gluteus medius tear diagnosed?
Diagnosis of a gluteus medius tear begins with a thorough physical examination by an orthopedic specialist. Your doctor will ask about your symptoms, when they started, and what activities make them worse. During the physical exam, they’ll perform specific tests including the Trendelenburg test, where you stand on one leg to see if your hip drops on the opposite side, indicating weakness.
The doctor will also assess tenderness by palpating the area around your hip and may perform a straight leg raise test, moving your leg away from your body to identify the exact location of pain and weakness. An MRI is typically the most useful imaging study for confirming a gluteus medius tear, as it provides detailed images of soft tissue and can reveal whether the tendon is stretched, partially torn, or completely ruptured. X-rays may also be taken to rule out bone-related issues like fractures or arthritis.
The MRI results help your doctor determine the extent of damage and plan the most appropriate treatment approach, whether conservative care or surgical repair.
Can a gluteus medius tear heal without surgery?
Yes, many gluteus medius tears can heal without surgery, particularly mild to moderate tears where the tendon remains partially intact. Conservative treatment typically includes several days of rest to reduce inflammation, followed by a comprehensive physical therapy program lasting 3-6 months.
Your treatment plan will likely include anti-inflammatory medications to manage pain and swelling, corticosteroid injections into the hip bursa for more significant pain relief, and ice or ultrasound therapy to calm inflammation. Physical therapy progresses through stages: first addressing pain and inflammation, then focusing on gentle stretching to restore flexibility and blood flow, and finally incorporating strengthening exercises to rebuild muscle stability. Most patients see significant improvement within 3-6 months of conservative treatment.
However, surgery becomes necessary when the tendon is completely torn or permanently lengthened, when conservative treatment fails to provide relief after 3-6 months, or when you continue to experience severe pain and functional limitations that impact your daily life. Your orthopedic specialist will monitor your progress and help determine if surgery is needed.
What is the recovery time after gluteus medius tear surgery?
Recovery from gluteus medius tear surgery varies depending on whether you have arthroscopic or open surgery, but expect a commitment of at least 6 months for full recovery. Immediately after surgery, you’ll need to use crutches or a hip stabilizing device to protect the repaired tendon from stretching. Physical therapy typically begins within 2-3 weeks after surgery, starting with gentle stretching exercises to prevent stiffness and scar tissue formation while maintaining your range of motion. For the first 6-8 weeks, you’ll focus on protected weight-bearing and gentle movements.
After 2-3 months, you’ll progress to more intensive strengthening exercises to rebuild muscle mass and hip stability. Most patients can return to light daily activities within 6-8 weeks, but full recovery with return to sports and strenuous activities typically takes 4-6 months or longer. Arthroscopic surgery generally offers faster recovery than open surgery, which requires more extensive tissue healing and intensive physical therapy.
Following your surgeon’s post-operative protocol and attending all physical therapy sessions is crucial for optimal healing and preventing re-injury to the weakened tendon.









